A vasovagal event, also known as vasovagal syncope, is a temporary loss of consciousness that occurs due to a sudden drop in blood pressure and a slowed heart rate. It is a common type of fainting episode that can be triggered by various factors. Understanding the basics of a vasovagal event can help individuals recognize the symptoms, identify potential triggers, and seek appropriate medical attention.
Understanding the Basics of a Vasovagal Event
Definition and Overview of Vasovagal Syncope
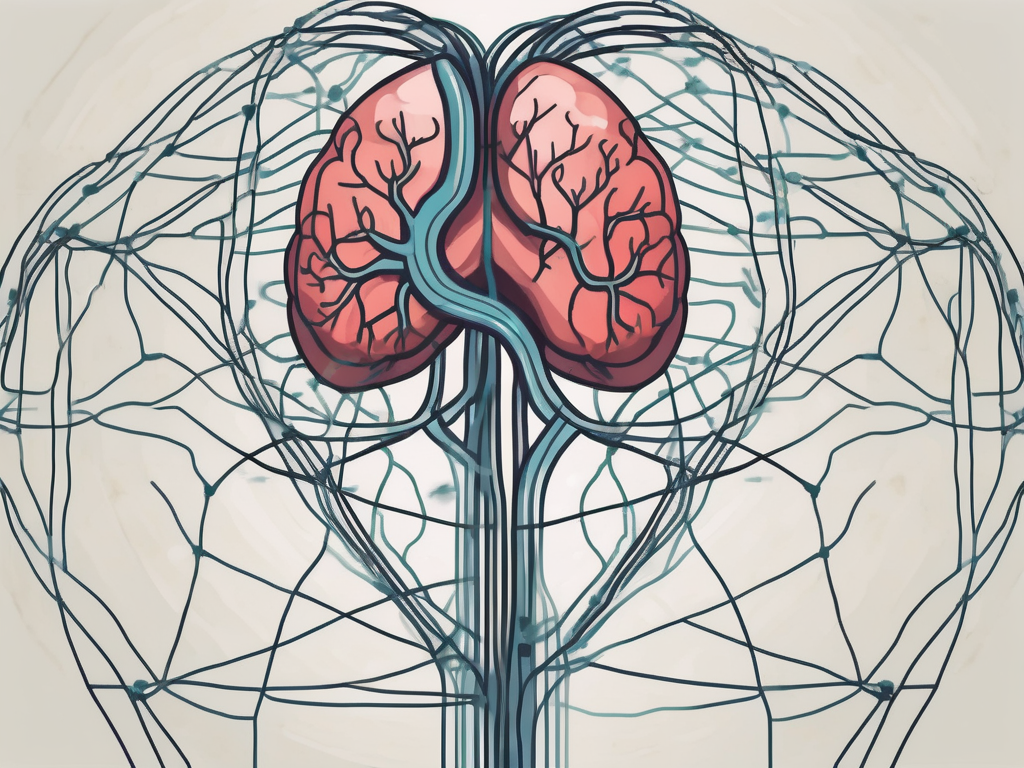
Vasovagal syncope is a type of fainting episode that occurs when the body overreacts to certain triggers, causing the heart rate and blood pressure to decrease suddenly. This reaction is primarily mediated by the vagus nerve, which plays a significant role in the body’s autonomic nervous system.
The autonomic nervous system controls various involuntary bodily functions, including heart rate, blood pressure, digestion, and sweating. In the case of a vasovagal event, an abnormal response by the autonomic nervous system leads to a cascade of physiological changes that ultimately cause fainting.
During a vasovagal event, the body’s response can be triggered by various factors. These triggers can include emotional stress, pain, standing for long periods, or even the sight of blood. When exposed to these triggers, the autonomic nervous system reacts by sending signals through the vagus nerve to slow down the heart rate and dilate blood vessels. This sudden drop in blood pressure and heart rate can result in fainting.
The Role of the Vagus Nerve in the Body
The vagus nerve, also known as the tenth cranial nerve, is one of the most crucial components of the autonomic nervous system. It originates in the brainstem and extends throughout the body, innervating various organs and tissues.
In relation to vasovagal syncope, the vagus nerve acts as a communication pathway between the brain and the heart. It carries signals that regulate heart rate, blood pressure, and other cardiovascular functions. Under normal circumstances, these signals are finely balanced to maintain stability. However, in certain situations, the vagus nerve can become overstimulated, leading to a vasovagal event.
Understanding the intricate workings of the vagus nerve is essential in comprehending the mechanisms behind vasovagal syncope. The vagus nerve consists of both sensory and motor fibers, allowing it to transmit information from the body to the brain and vice versa. This bidirectional communication enables the body to respond to various stimuli and maintain homeostasis.
When a trigger for vasovagal syncope is encountered, the vagus nerve responds by releasing neurotransmitters that inhibit the heart’s electrical activity and relax the blood vessels. This response aims to reduce the body’s overall metabolic demand and redirect blood flow to vital organs, such as the brain. However, in some cases, this response becomes exaggerated, leading to a sudden and significant drop in blood pressure, resulting in fainting.
It is important to note that vasovagal syncope is a relatively common condition and is typically harmless. However, in certain situations, such as when fainting occurs while driving or operating heavy machinery, it can pose a significant risk. Therefore, understanding the triggers and mechanisms behind vasovagal events can help individuals manage and prevent such episodes effectively.
The Physiology Behind a Vasovagal Event
The Body’s Response to Stress and Fear
Stress and fear can trigger a vasovagal event in susceptible individuals. When faced with a stressful or fearful situation, the body undergoes a complex physiological response commonly known as the fight-or-flight response. This response involves the release of stress hormones, increased heart rate, and elevated blood pressure to prepare the body for action.
However, in the case of a vasovagal event, the body’s response is quite the opposite. Instead of an increased heart rate and blood pressure, there is a sudden drop in both. This response occurs due to excessive stimulation of the vagus nerve, which overrides the body’s normal fight-or-flight response.
During a vasovagal event, the body experiences a cascade of physiological changes. As stress or fear triggers the response, the brain sends signals to the hypothalamus, a small region at the base of the brain responsible for regulating various bodily functions. The hypothalamus then activates the sympathetic nervous system, which releases stress hormones like adrenaline into the bloodstream.
Adrenaline, also known as epinephrine, acts as a powerful stimulant, increasing heart rate and blood pressure. This surge in cardiovascular activity prepares the body for action, enabling it to respond quickly to potential threats. At the same time, blood vessels constrict, redirecting blood flow to vital organs and muscles, ensuring they receive an adequate supply of oxygen and nutrients.
The Connection Between the Heart and the Vagus Nerve
The heart and the vagus nerve share an intricate relationship. The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and branches out to various organs, including the heart, lungs, and digestive system.
The vagus nerve controls the heart’s rate and rhythm, ensuring that it beats at an appropriate speed to meet the body’s needs. It does this by releasing neurotransmitters that either speed up or slow down the heart’s electrical activity. When the body is in a state of rest or relaxation, the vagus nerve predominates, slowing down the heart rate and promoting a sense of calm.
In a vasovagal event, the vagus nerve releases excessive amounts of these neurotransmitters, causing the heart rate to slow down drastically. This sudden drop in heart rate, known as bradycardia, can lead to a decrease in blood flow to the brain. Additionally, the vagus nerve also triggers the dilation of blood vessels, resulting in reduced blood flow to the brain.
As blood flow to the brain decreases, the brain’s oxygen supply is compromised. This lack of oxygen can cause dizziness, lightheadedness, and ultimately, a temporary loss of consciousness. The body’s response to the vasovagal event is an adaptive mechanism, aiming to protect the brain from potential harm by reducing its metabolic demands.
It is important to note that while vasovagal events can be triggered by stress and fear, they can also occur in response to other stimuli, such as pain, standing for prolonged periods, or even the sight of blood. Understanding the physiology behind these events can help individuals recognize the warning signs and take appropriate measures to prevent or manage them.
Symptoms and Signs of a Vasovagal Event
Physical Manifestations of a Vasovagal Syncope
Several physical symptoms may be experienced before, during, and after a vasovagal event. These can vary from person to person but commonly include:
- Dizziness or lightheadedness
- Blurred vision
- Nausea
- Pale skin
- Cold sweat
It is important to note that these symptoms typically resolve once the individual regains consciousness. However, medical evaluation is necessary to rule out any underlying conditions that may be contributing to the syncope episodes.
When a vasovagal event occurs, the body’s autonomic nervous system responds by causing a sudden drop in blood pressure and heart rate. This can lead to a decrease in blood flow to the brain, resulting in the physical symptoms mentioned above. Dizziness or lightheadedness is often one of the first signs experienced, as the brain is deprived of oxygen-rich blood.
Blurred vision is another common symptom, as the eyes rely on a steady blood supply to function properly. When blood flow is compromised during a vasovagal event, the eyes may struggle to focus, leading to temporary vision disturbances.
Nausea is also frequently reported during a vasovagal event. The sudden drop in blood pressure can affect the digestive system, causing discomfort and a feeling of queasiness. This can be further exacerbated by the body’s stress response, which can trigger the release of stomach acid.
As blood flow to the skin is reduced during a vasovagal event, the individual may appear pale. This is due to vasoconstriction, a narrowing of the blood vessels, which limits blood flow to the surface of the skin. Additionally, the body may produce cold sweat as a result of the autonomic nervous system’s attempt to regulate body temperature.
It is crucial to seek medical evaluation after experiencing a vasovagal event to ensure that there are no underlying conditions contributing to the syncope episodes. A healthcare professional can conduct a thorough assessment, which may include a physical examination, blood tests, and further diagnostic procedures, if necessary.
Emotional and Psychological Symptoms
Alongside the physical manifestations, individuals experiencing a vasovagal event may also exhibit emotional and psychological symptoms. These can include anxiety, fear, confusion, and a sense of impending doom. These emotional responses are often a result of the sudden loss of consciousness and can have a profound impact on the individual’s well-being.
The experience of a vasovagal event can be distressing and overwhelming, leading to heightened emotional responses. Anxiety and fear may arise from the uncertainty and unpredictability of the episodes, as well as the potential embarrassment or inconvenience they may cause. Confusion can occur as the individual tries to make sense of what happened during the period of unconsciousness, while a sense of impending doom may stem from the perceived threat to their safety and well-being.
If you or someone you know frequently experiences vasovagal events, it is advisable to consult with a healthcare professional for further evaluation and guidance. They can provide support, education, and potential treatment options to help manage the physical and emotional symptoms associated with vasovagal syncope.
Causes and Triggers of Vasovagal Events
Vasovagal events, also known as vasovagal syncope, can be triggered by a variety of situations. Understanding these potential triggers is important as it allows individuals to avoid or manage situations that may result in a vasovagal event.
Common Situations Leading to Vasovagal Syncope
One common trigger for vasovagal events is exposure to blood or needles. This can be particularly challenging for individuals who have a fear of needles or a phobia of blood. The sight or thought of blood, or the process of getting an injection, can cause a sudden drop in blood pressure and heart rate, leading to a vasovagal event.
Prolonged standing or being in an upright position for an extended period of time can also trigger a vasovagal event. This is because staying in an upright position for too long can cause blood to pool in the lower extremities, leading to a decrease in blood flow to the brain. As a result, dizziness, lightheadedness, and even fainting can occur.
Extreme heat or crowded environments can also contribute to vasovagal events. In hot weather, the body tries to cool itself down by dilating blood vessels near the skin’s surface, which can lead to a drop in blood pressure. Similarly, being in a crowded environment can cause feelings of anxiety or claustrophobia, which can trigger a vasovagal response.
Emotional distress or anxiety is another common trigger for vasovagal events. Stressful situations, panic attacks, or overwhelming emotions can activate the body’s fight-or-flight response, causing a surge of adrenaline and a subsequent drop in blood pressure.
It is important to note that triggers can vary from person to person. What may cause a vasovagal event in one individual may not affect another in the same way. Identifying specific triggers may require medical expertise and a thorough evaluation of an individual’s medical history.
Underlying Health Conditions and Vasovagal Events
In some cases, vasovagal syncope may be associated with underlying health conditions. These conditions can include heart conditions, such as arrhythmias or structural abnormalities, as well as neurological disorders.
Heart conditions, such as an irregular heartbeat (arrhythmia), can disrupt the normal electrical signals that regulate the heart’s rhythm. This can lead to a sudden drop in blood pressure and trigger a vasovagal event. Structural abnormalities, such as valve disorders or congenital heart defects, can also contribute to the occurrence of vasovagal events.
Neurological disorders, such as epilepsy or migraines, can also be linked to vasovagal events. These conditions can affect the autonomic nervous system, which controls involuntary bodily functions like blood pressure and heart rate. When the autonomic nervous system is disrupted, it can result in a vasovagal response.
If you experience recurrent vasovagal events or have concerns about your health, it is strongly recommended to consult with a healthcare professional. They can evaluate your symptoms, perform necessary tests, and provide appropriate guidance and treatment. A comprehensive medical evaluation is essential to determine if any underlying conditions contribute to the frequency or severity of vasovagal events.
Diagnosis and Treatment of Vasovagal Syncope
Vasovagal syncope, also known as fainting or a vasovagal episode, is a common condition that occurs when there is a sudden drop in blood pressure and heart rate, leading to a temporary loss of consciousness. While the exact cause of vasovagal syncope is not fully understood, it is believed to be triggered by certain factors such as emotional stress, pain, dehydration, or standing for long periods.
Medical Tests for Identifying Vasovagal Events
Diagnosing vasovagal syncope typically involves a thorough medical history evaluation, physical examination, and specific tests. These tests are essential in confirming the diagnosis and ruling out other potential causes for the fainting episodes.
One of the primary tests used is an electrocardiogram (ECG), which assesses the heart’s rhythm and rate. By analyzing the electrical activity of the heart, doctors can identify any abnormalities that may contribute to vasovagal syncope.
In addition to an ECG, a tilt-table test may be conducted to provoke and evaluate vasovagal events. During this test, the patient lies on a table that is slowly tilted to an upright position. This change in position can trigger a vasovagal response, allowing doctors to observe the symptoms and monitor changes in blood pressure and heart rate.
Blood tests may also be performed to rule out other underlying conditions that could be causing the fainting episodes. These tests help doctors eliminate possibilities such as anemia, low blood sugar, or thyroid problems, which can mimic the symptoms of vasovagal syncope.
Treatment Options and Lifestyle Changes
The treatment of vasovagal syncope varies depending on the underlying cause, severity, and impact on an individual’s daily life. Treatment options may include a combination of lifestyle modifications, medications, vagal maneuvers, and, in certain cases, implantable devices.
Lifestyle modifications play a crucial role in managing vasovagal syncope. Patients are advised to identify and avoid triggers that may induce fainting episodes. These triggers can vary from person to person but may include prolonged standing, extreme heat, crowded places, or emotional stress. Staying hydrated and maintaining a regular sleep schedule are also recommended to help regulate blood pressure and reduce the frequency of syncope episodes.
Medications can be prescribed to control heart rate and blood pressure, helping to prevent the sudden drops that lead to fainting. Beta-blockers, for example, are commonly used to slow the heart rate and stabilize blood pressure levels. Other medications, such as fludrocortisone, may be prescribed to increase blood volume and improve circulation.
Vagal maneuvers are physical techniques that stimulate the vagus nerve, which plays a role in regulating heart rate and blood pressure. These maneuvers can be performed during the onset of symptoms to help restore normal blood flow and prevent syncope. The Valsalva maneuver, for instance, involves forcefully exhaling against a closed airway, increasing pressure in the chest and stimulating the vagus nerve.
In certain cases, implantable devices like pacemakers may be recommended to regulate heart rhythm and prevent syncope. These devices continuously monitor the heart’s electrical activity and deliver electrical impulses when necessary to maintain a stable heart rate.
It is important to note that treatment decisions should be made in consultation with a healthcare professional who can provide personalized recommendations based on individual circumstances. With proper diagnosis and management, individuals with vasovagal syncope can lead fulfilling lives with a reduced risk of fainting episodes.
Living with Vasovagal Syncope
Coping Mechanisms and Strategies
Coping with vasovagal syncope involves adopting strategies to minimize the risk of fainting episodes and manage associated symptoms. Some helpful suggestions include:
- Increasing fluid intake to maintain hydration
- Avoiding triggers, such as prolonged standing or exposure to triggering environments
- Practicing stress management techniques, such as deep breathing exercises or mindfulness meditation
- Wearing compression stockings to improve blood flow
Implementing these coping mechanisms can significantly improve an individual’s quality of life and reduce the frequency of vasovagal events. However, it is crucial to remember that these strategies may not be applicable to everyone and consulting with a healthcare professional is essential for personalized guidance.
The Impact on Daily Life and Activities
Vasovagal syncope can have a significant impact on daily life and activities, affecting an individual’s physical, emotional, and social well-being. Fainting episodes may lead to concerns about safety, limitations in mobility or independence, and increased anxiety or fear.
It is important to seek support from healthcare professionals, family, and friends to navigate these challenges. Additionally, joining support groups or connecting with others who have experienced similar situations can provide valuable insights and emotional support.
In conclusion, understanding the basics of a vasovagal event is crucial for individuals who experience fainting episodes or know someone who does. Recognizing the symptoms, identifying triggers, and seeking appropriate medical attention can help manage vasovagal syncope and improve the overall quality of life. If you or someone you know is impacted by vasovagal events, it is recommended to consult with a healthcare professional for a comprehensive evaluation and guidance tailored to individual needs.