Having a vasovagal episode can be a scary and unsettling experience. Understanding what causes these episodes can help individuals better manage and cope with this condition. In this article, we will explore the various factors that contribute to vasovagal episodes and provide insights into the physiology behind them.
Understanding Vasovagal Syncope
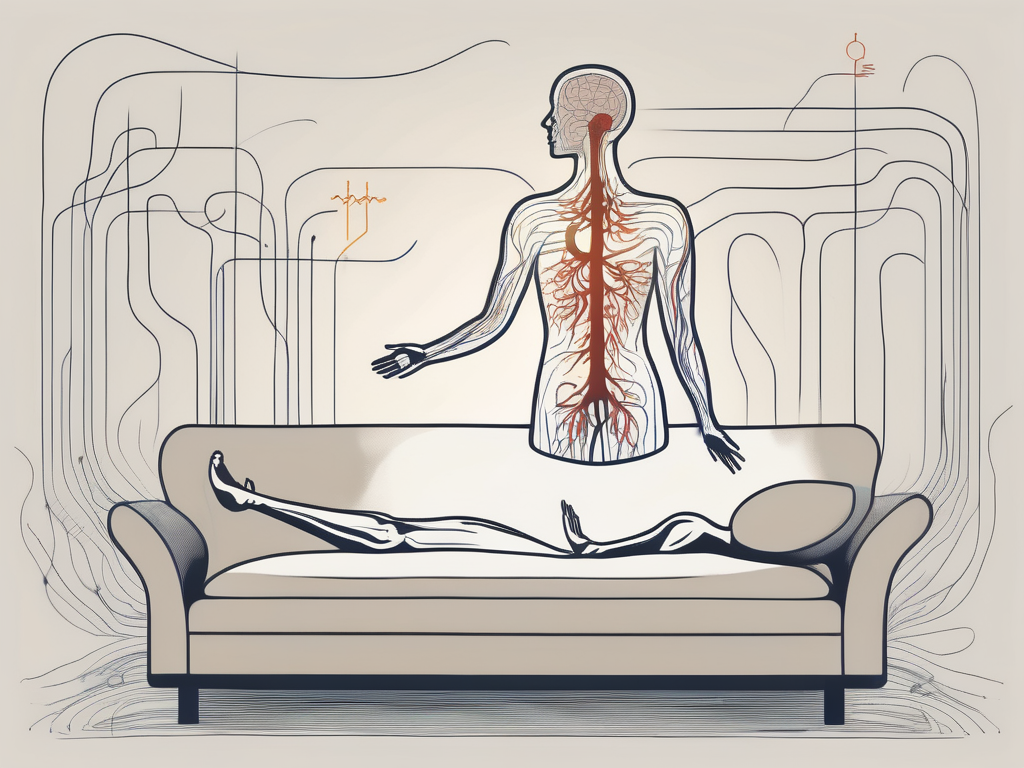
Vasovagal syncope, also known as vasovagal episodes or neurocardiogenic syncope, is a common form of fainting. It occurs when there is an overstimulation of the vagus nerve, leading to a sudden drop in blood pressure and heart rate. This, in turn, causes a temporary disruption in blood flow to the brain, resulting in a loss of consciousness.
Definition and Overview of Vasovagal Syncope
Vasovagal syncope is a self-limiting condition characterized by sudden fainting episodes. It is often triggered by specific stimuli, such as stress, pain, or emotional distress. While vasovagal episodes may be alarming, they are generally harmless and do not indicate a serious underlying health problem.
The Role of the Vagus Nerve in the Body
The vagus nerve, also known as the cranial nerve X, plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, digestion, and breathing. It consists of a network of nerves that extends from the brainstem to different organs throughout the body. The overstimulation of the vagus nerve is what triggers vasovagal episodes.
When the vagus nerve is overstimulated, it sends signals to the brain that result in a cascade of physiological responses. One of the key responses is the dilation of blood vessels, which causes blood pressure to drop. Additionally, the vagus nerve also slows down the heart rate, further contributing to the decrease in blood flow to the brain.
While the exact mechanisms behind the overstimulation of the vagus nerve in vasovagal syncope are not fully understood, several triggers have been identified. Emotional stress, such as anxiety or fear, can activate the vagus nerve and lead to a fainting episode. Similarly, experiencing pain, whether it be from an injury or a medical procedure, can also stimulate the vagus nerve and trigger syncope.
Furthermore, certain environmental factors can contribute to the occurrence of vasovagal syncope. Standing for long periods, especially in hot and crowded places, can cause blood to pool in the legs and lower the overall blood volume in the body. This, in turn, increases the likelihood of vagus nerve activation and subsequent fainting.
It is worth noting that while vasovagal syncope is generally a benign condition, it can still have an impact on an individual’s quality of life. Fainting episodes can be unpredictable and may occur in inconvenient or potentially dangerous situations. As a result, individuals with vasovagal syncope may need to take precautions, such as avoiding triggers and ensuring they are in a safe environment when an episode occurs.
In conclusion, vasovagal syncope is a common form of fainting that occurs due to the overstimulation of the vagus nerve. While the exact mechanisms behind this condition are not fully understood, triggers such as stress, pain, and environmental factors have been identified. Although vasovagal episodes are generally harmless, they can still have an impact on an individual’s daily life. Understanding the role of the vagus nerve and the various triggers can help individuals manage and cope with vasovagal syncope effectively.
The Triggers of Vasovagal Episodes
Vasovagal episodes can be triggered by a wide range of factors. These triggers can vary from person to person, making it important for individuals to identify and avoid their specific triggers to reduce the frequency of episodes.
Emotional Triggers
Strong emotions, such as fear, anxiety, stress, or even excitement, can prompt vasovagal episodes in susceptible individuals. The body’s response to these intense emotions can cause a sudden decrease in blood pressure and heart rate, leading to fainting.
For example, imagine a person with a fear of public speaking. As they step onto the stage to deliver a speech, their heart starts racing, and their palms become sweaty. These physical manifestations of anxiety can trigger a vasovagal episode, causing them to faint in front of the audience.
Similarly, individuals who experience extreme excitement, such as winning a competitive sports event or receiving surprising news, may also be at risk of vasovagal episodes. The surge of adrenaline and the subsequent drop in blood pressure can result in a sudden loss of consciousness.
Physical Triggers
Physical factors, such as prolonged standing, standing up too quickly after sitting or lying down, or straining during bowel movements, can trigger vasovagal episodes. These actions exert pressure on the blood vessels, leading to a temporary drop in blood flow to the brain.
Consider a scenario where a person has been standing for an extended period, such as waiting in line for hours. The constant pressure on their legs can impede blood circulation, causing a vasovagal episode. This is why it is crucial for individuals who are prone to these episodes to take frequent breaks and avoid prolonged periods of standing.
In addition, sudden changes in posture, such as getting up quickly from a lying or sitting position, can also trigger vasovagal episodes. When the body rapidly adjusts to a new position, the blood vessels may struggle to adapt, leading to a momentary decrease in blood flow to the brain.
Environmental Triggers
Environmental factors, such as hot and crowded spaces, extreme temperatures, or the sight of blood, can also induce vasovagal episodes. These triggers can intensify the body’s response to stress and lead to fainting.
Imagine a person attending a packed concert on a scorching summer day. The combination of the heat and the crowded environment can cause the body to overheat, leading to a vasovagal episode. Similarly, exposure to extremely cold temperatures can trigger a similar response, as the body tries to preserve heat by constricting blood vessels, resulting in a sudden drop in blood pressure.
Furthermore, the sight of blood or other distressing medical procedures can elicit a strong emotional response in some individuals, leading to vasovagal episodes. This is commonly observed in people who have a fear or phobia of needles or medical procedures. The anxiety and stress associated with these situations can trigger a vasovagal response, causing them to faint.
In conclusion, vasovagal episodes can be triggered by various factors, including emotional, physical, and environmental triggers. It is crucial for individuals who experience these episodes to identify and avoid their specific triggers to minimize the risk of fainting and ensure their well-being.
The Physiology Behind Vasovagal Episodes
Vasovagal episodes involve a complex interplay of physiological responses within the body. Understanding the underlying mechanisms can shed light on why certain triggers result in fainting.
The Body’s Response to Triggers
When faced with a trigger, the body’s stress response system, known as the fight-or-flight response, is activated. This response is a survival mechanism that prepares the body to either confront the threat or flee from it. The activation of the fight-or-flight response involves the release of stress hormones, such as adrenaline and cortisol, into the bloodstream.
For individuals prone to vasovagal syncope, this stress response may become exaggerated. The exaggerated response can be triggered by various factors, including emotional stress, pain, fear, or even the sight of blood. When these triggers are encountered, the body’s stress response system goes into overdrive, leading to a cascade of physiological changes.
The Drop in Blood Pressure and Heart Rate
As a result of the exaggerated stress response, the heart rate slows down, and blood vessels dilate. The slowing of the heart rate is known as bradycardia, and the dilation of blood vessels is called vasodilation. These changes in heart rate and blood vessel diameter can cause a rapid decline in blood pressure.
When blood pressure drops significantly, the brain may not receive an adequate supply of oxygen and nutrients. This lack of blood flow to the brain can trigger fainting and loss of consciousness. Fainting, also known as syncope, is the body’s way of protecting the brain by temporarily reducing its energy demands.
During a vasovagal episode, the brain’s autonomic control centers, which regulate involuntary bodily functions, become temporarily disrupted. This disruption can lead to a loss of consciousness, as the brain is unable to maintain normal control over vital functions such as heart rate and blood pressure.
It is important to note that while vasovagal episodes can be alarming, they are generally not life-threatening. Most episodes are self-limiting and resolve on their own once the trigger is removed or the individual lies down, allowing blood flow to return to the brain.
Overall, the physiology behind vasovagal episodes involves a complex interplay of the body’s stress response system, heart rate, blood pressure, and autonomic control centers in the brain. By understanding these mechanisms, healthcare professionals can better manage and treat individuals who experience recurrent vasovagal episodes.
Symptoms and Signs of a Vasovagal Episode
Recognizing the symptoms and signs associated with a vasovagal episode is essential for both individuals experiencing these events and those around them. Understanding the warning signs can help prevent injury and ensure a safe and supportive environment.
A vasovagal episode, also known as vasovagal syncope, is a sudden drop in heart rate and blood pressure that leads to a temporary loss of consciousness. It is a common condition that can occur in response to various triggers, such as emotional stress, pain, or standing for long periods.
While the exact cause of vasovagal episodes is not fully understood, it is believed to involve an overstimulation of the vagus nerve, which regulates heart rate and blood pressure. This overstimulation can lead to a sudden decrease in blood flow to the brain, resulting in the symptoms experienced during an episode.
Pre-Syncope Symptoms
Pre-syncope symptoms occur before an individual loses consciousness. These symptoms may include lightheadedness, nausea, feeling warm or cold, blurred vision, or a sudden sense of fatigue. These warning signs serve as an alert that a vasovagal episode may be imminent, allowing individuals to take appropriate measures to prevent injury.
It is important to note that not everyone experiences the same pre-syncope symptoms. Some individuals may only have a few mild warning signs, while others may experience a combination of symptoms that are more severe.
During the Episode
During a vasovagal episode, an individual may experience pale skin, loss of muscle control, shallow breathing, and, ultimately, a temporary loss of consciousness. The loss of consciousness is usually brief, lasting only a few seconds to a couple of minutes.
It is essential to keep the person safe by gently lowering them to the ground to prevent injury. Placing a pillow or cushion under their head can provide additional comfort and support. It is important not to try to wake the person up forcefully, as they will regain consciousness on their own.
While witnessing someone go through a vasovagal episode can be distressing, it is crucial to remain calm and reassure the person once they regain consciousness. Offering them water and helping them sit up slowly can aid in their recovery.
Post-Syncope Symptoms
After regaining consciousness, individuals may experience confusion, dizziness, headache, and fatigue. These post-syncope symptoms are a normal part of the recovery process and usually resolve within a short period.
It is crucial to allow the person time to recover and rest following a vasovagal episode. Encouraging them to lie down and elevate their legs can help improve blood flow and alleviate any lingering symptoms.
In some cases, individuals may require medical attention if their symptoms persist or if they injure themselves during the episode. It is always advisable to consult a healthcare professional for a proper evaluation and guidance on managing vasovagal episodes.
By understanding the symptoms and signs associated with a vasovagal episode, individuals can take appropriate measures to prevent injury and create a supportive environment for those experiencing these events. Education and awareness play a vital role in ensuring the well-being of individuals affected by vasovagal syncope.
Diagnosis and Treatment of Vasovagal Syncope
Diagnosing vasovagal syncope involves a comprehensive medical evaluation and ruling out underlying health conditions that may contribute to fainting episodes. Treatment options focus on avoiding triggers and making lifestyle changes.
Vasovagal syncope, also known as neurocardiogenic syncope, is a common cause of fainting episodes. It occurs when there is a sudden drop in blood pressure and heart rate, leading to a temporary loss of consciousness. While vasovagal syncope is generally not life-threatening, it can be a cause of concern for individuals who experience recurrent episodes.
Medical Evaluation and Diagnosis
An accurate diagnosis is crucial to differentiate vasovagal syncope from other forms of syncope with potentially serious underlying causes. Medical professionals may conduct various tests, such as electrocardiograms (ECGs), tilt table tests, or event monitors to assess heart function and identify any abnormalities.
During an ECG, electrodes are placed on the chest, arms, and legs to record the electrical activity of the heart. This test can help detect any irregularities in heart rhythm or conduction that may contribute to fainting episodes. Tilt table tests involve lying on a table that is tilted to different angles while heart rate and blood pressure are monitored. This test helps provoke vasovagal syncope symptoms and aids in diagnosis. Event monitors are portable devices that record heart rhythm over an extended period, allowing doctors to capture any abnormalities that may occur during fainting episodes.
In addition to these tests, medical professionals will also take a detailed medical history and perform a physical examination to rule out any underlying health conditions that may contribute to vasovagal syncope. This may include checking blood pressure, conducting blood tests, and evaluating the overall cardiovascular health of the patient.
Treatment Options and Lifestyle Changes
The primary approach to managing vasovagal syncope involves identifying and avoiding triggers. Triggers can vary from person to person but commonly include prolonged standing, emotional stress, dehydration, and hot environments. By recognizing and avoiding these triggers, individuals can significantly reduce the frequency of fainting episodes.
Practicing stress-reduction techniques, such as deep breathing exercises, meditation, or yoga, can help manage emotional stress and prevent vasovagal syncope episodes. Adequate hydration is also essential, as dehydration can contribute to low blood pressure and increase the likelihood of fainting. It is recommended to drink plenty of fluids throughout the day, especially in hot weather or during physical activity.
In some cases, medications may be prescribed to help regulate blood pressure and prevent vasovagal syncope episodes. These medications may include beta-blockers, which slow down the heart rate, or selective serotonin reuptake inhibitors (SSRIs), which can help manage anxiety and stress. Compression stockings, which apply pressure to the lower extremities, can also be beneficial in preventing blood pooling and maintaining adequate blood flow.
Furthermore, making certain lifestyle changes can have a positive impact on managing vasovagal syncope. These changes may include maintaining a balanced diet, avoiding excessive alcohol or caffeine consumption, and getting regular exercise. A well-balanced diet ensures proper nutrition and can help stabilize blood pressure. Limiting alcohol and caffeine intake can prevent dehydration and minimize the risk of triggering syncope episodes. Regular exercise, under the guidance of a healthcare professional, can improve cardiovascular health and reduce the frequency of fainting episodes.
In conclusion, the diagnosis and treatment of vasovagal syncope require a comprehensive medical evaluation to rule out underlying health conditions and identify triggers. By implementing lifestyle changes and following the recommended treatment options, individuals with vasovagal syncope can effectively manage their condition and reduce the occurrence of fainting episodes.
Living with Vasovagal Syncope
While vasovagal syncope can be disruptive and unsettling, individuals can take steps to manage their condition effectively and enhance their quality of life.
Coping Mechanisms and Strategies
Developing coping mechanisms and strategies can play a significant role in managing vasovagal episodes. This may involve learning stress management techniques, practicing deep breathing exercises, and adopting relaxation techniques, such as yoga or meditation. It may also be beneficial for individuals to share their experiences and seek support from others with similar conditions.
Long-Term Prognosis and Quality of Life
Most individuals with vasovagal syncope lead normal lives and have an excellent long-term prognosis. By identifying and managing triggers, individuals can significantly reduce the frequency of episodes and improve their overall quality of life. However, it is essential to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
Conclusion
In conclusion, vasovagal syncope can be frightening, but understanding its causes can help individuals navigate this condition. By recognizing triggers, managing stress, and making necessary lifestyle changes, individuals can effectively reduce the frequency and severity of vasovagal episodes. However, it is crucial to consult with a healthcare professional for proper diagnosis, advice, and guidance on the best course of action.