The vasovagal response, also known as vasovagal syncope, is a common condition that affects many individuals. Understanding what happens in a vasovagal response can help individuals recognize and manage this condition effectively. In this article, we will delve into the various aspects of a vasovagal response and address its physiological mechanisms, symptoms, diagnosis, treatment options, and strategies for living with it.
Understanding the Vasovagal Response
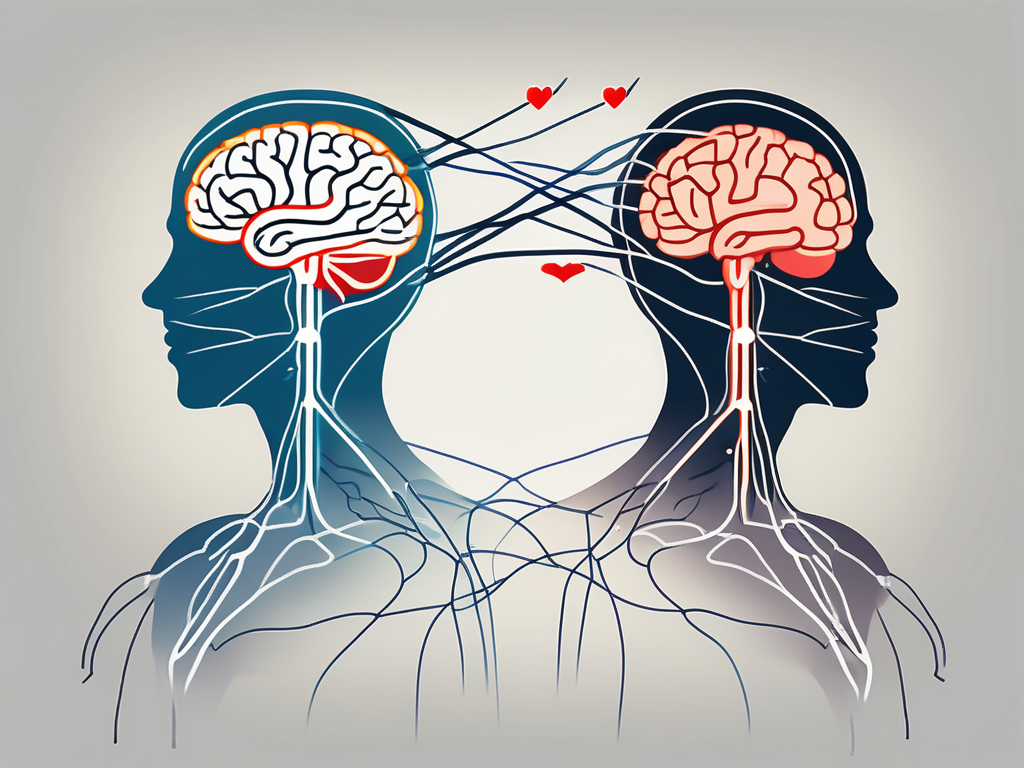
A vasovagal response is a type of reflex reaction that occurs when the body overreacts to certain triggers, leading to a sudden drop in heart rate and blood pressure. This reaction is mediated by the vagus nerve, a key player in our autonomic nervous system. The vagus nerve is responsible for regulating vital functions such as heart rate, blood pressure, and digestion. When the vagus nerve is stimulated, it can cause a cascade of events resulting in a vasovagal response.
The Role of the Vagus Nerve
The vagus nerve acts as the messenger between the brain and various organs, including the heart and blood vessels. It is the longest cranial nerve in the body, extending from the brainstem to the abdomen. This extensive reach allows the vagus nerve to influence a wide range of bodily functions.
During a vasovagal response, the vagus nerve becomes overstimulated, sending signals to the heart to slow down and the blood vessels to dilate. This intricate communication system ensures that the body can adapt to different situations, maintaining homeostasis and responding appropriately to external stimuli.
Furthermore, the vagus nerve is not only responsible for the vasovagal response but also plays a crucial role in regulating digestion. It stimulates the release of digestive enzymes and controls the movement of food through the gastrointestinal tract. This dual function highlights the complexity and importance of the vagus nerve in maintaining overall bodily function.
The Body’s Reaction to Stress and Fear
The vasovagal response is often triggered by stress, fear, or extreme emotions. When faced with a stressful situation or confronted with fear, the body’s natural response is to activate the fight-or-flight response. This physiological reaction prepares the body for action, increasing heart rate and blood pressure.
However, in some individuals, the vagus nerve overreacts and triggers a vasovagal response instead. This reaction is thought to be an evolutionary mechanism designed to protect the body from potentially harmful stressors. By causing a sudden drop in heart rate and blood pressure, the body conserves energy and redirects blood flow to vital organs, such as the brain.
Interestingly, the vasovagal response is not limited to stressful or fearful situations. It can also be triggered by various other factors, including pain, standing up too quickly, or even the sight of blood. These triggers can activate the vagus nerve, leading to a vasovagal response and subsequent fainting.
It is important to note that while the vasovagal response is generally harmless, it can be a cause for concern in certain situations. For example, if an individual faints and injures themselves during a vasovagal episode, medical attention may be required to address any injuries sustained.
In conclusion, the vasovagal response is a fascinating reflex reaction mediated by the vagus nerve. It serves as a protective mechanism, allowing the body to adapt to various stressors and maintain overall homeostasis. Understanding this response can help individuals recognize and manage triggers, ensuring their well-being and safety.
The Physiology of a Vasovagal Response
To better understand what happens during a vasovagal response, it is important to explore the physiological mechanisms at play.
When a person experiences a vasovagal response, their body undergoes a series of intricate physiological changes. These changes are triggered by various factors that can differ from person to person.
The Triggering Factors
Various factors can trigger a vasovagal response in susceptible individuals. Common triggers include prolonged standing, heat exposure, dehydration, pain, emotional stress, and the sight of blood or needles. Identifying personal triggers can help individuals take steps to minimize the risk of experiencing a vasovagal response.
For instance, prolonged standing can lead to blood pooling in the lower extremities, which can activate the vasovagal response. Heat exposure can cause blood vessels to dilate, leading to a drop in blood pressure. Dehydration can also contribute to a vasovagal response as it reduces blood volume, making it harder for the heart to pump blood effectively. Pain, whether acute or chronic, can stimulate the vagus nerve and trigger a response. Emotional stress, such as anxiety or fear, can activate the body’s fight-or-flight response, which can then be followed by a vasovagal response. Lastly, the sight of blood or needles can trigger a strong emotional response, leading to a vasovagal reaction.
The Process of Fainting
During a vasovagal response, the body undergoes a series of physiological changes that ultimately lead to fainting. When triggered, the vagus nerve sends signals to slow down the heart rate and dilate blood vessels, causing a sudden drop in blood pressure. As a result, less oxygenated blood reaches the brain, leading to a temporary loss of consciousness. In most cases, individuals regain consciousness within seconds or minutes.
When the vagus nerve is activated, it releases acetylcholine, a neurotransmitter that acts as a natural brake on the heart. This causes the heart rate to slow down, reducing the amount of blood pumped out with each beat. At the same time, the blood vessels in the body dilate, allowing blood to pool in the legs and lower body. This pooling of blood further decreases the amount of blood available to be pumped to the brain.
The sudden drop in blood pressure and reduced blood flow to the brain result in a temporary loss of consciousness. This loss of consciousness is often accompanied by other symptoms such as lightheadedness, dizziness, blurred vision, and a feeling of warmth or sweating. These symptoms typically resolve once the individual is lying down and blood flow to the brain is restored.
It is important to note that while fainting during a vasovagal response can be alarming, it is generally not a cause for concern. Most individuals recover quickly and without any long-term effects. However, if fainting episodes become frequent or are accompanied by concerning symptoms, it is advisable to seek medical attention to rule out any underlying conditions.
Symptoms of the Vasovagal Response
Recognizing the symptoms of a vasovagal response is crucial for timely management and prevention. The symptoms can vary from person to person and may include a combination of physical and emotional manifestations.
When it comes to physical symptoms, there are several commonly associated with a vasovagal response. Lightheadedness is a prevalent symptom, making individuals feel as if they are about to faint. This sensation is often accompanied by dizziness, making it difficult to maintain balance. Blurred vision is another physical symptom that can occur, making it challenging to see clearly. In addition, individuals may notice their skin becoming pale, a result of decreased blood flow to the surface of the body. Sweating is also common during a vasovagal response, as the body tries to regulate its temperature. Furthermore, individuals may experience nausea, adding to the discomfort they already feel. Lastly, a slow or weak pulse is often observed, indicating a decrease in heart rate.
Emotional symptoms are also experienced during a vasovagal response, and they can vary from person to person. Anxiety is a common emotional response, as individuals may feel a sense of unease or apprehension. Fear is another emotional symptom that can arise, as individuals may be frightened by the sudden onset of symptoms. Some individuals may even experience a sense of impending doom, which can be incredibly distressing. It is important to remember that emotions are highly individualized, and individuals may experience varying emotional responses during a vasovagal episode.
Diagnosis and Treatment of Vasovagal Response
Seeking medical evaluation is crucial if you suspect you are experiencing a vasovagal response. While this article provides valuable information, it is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
Medical Evaluation
A thorough medical evaluation is necessary to rule out other potential underlying causes for fainting episodes. When you visit your doctor, they will take a detailed medical history to understand your symptoms better. They may ask about your family history of fainting or any other related conditions. Additionally, your doctor may perform a physical examination, checking your blood pressure, heart rate, and listening to your heart and lungs. These tests will help determine if there are any other factors contributing to your fainting episodes.
In some cases, your doctor may order additional tests to confirm the diagnosis. Blood work can help identify any underlying medical conditions that may be causing your vasovagal response. An electrocardiogram (ECG) can provide information about your heart’s electrical activity and detect any abnormalities. Tilt table testing is another diagnostic tool that can help simulate fainting episodes to confirm the diagnosis of vasovagal response.
Therapeutic Approaches
Treatment for vasovagal response focuses on managing triggers and preventing fainting episodes. Lifestyle modifications can play a significant role in reducing the frequency of episodes. Staying hydrated is essential as dehydration can worsen symptoms. Your doctor may recommend drinking plenty of fluids, especially during hot weather or when engaging in physical activities.
Avoiding prolonged standing or sudden changes in posture can also help prevent fainting episodes. If you have a job that requires prolonged standing, your doctor may suggest taking regular breaks or using compression stockings to improve blood flow and prevent blood pooling in the legs.
In some cases, medications may be prescribed to regulate heart rate and maintain blood pressure. Beta-blockers are commonly used to slow down the heart rate and reduce the risk of fainting. Other medications, such as selective serotonin reuptake inhibitors (SSRIs), may be prescribed to help manage anxiety or panic attacks that can trigger vasovagal responses.
Your healthcare provider will determine the most appropriate treatment options based on your individual needs. It is essential to follow their guidance and attend regular follow-up appointments to monitor your progress and make any necessary adjustments to your treatment plan.
Living with Vasovagal Syncope
Living with vasovagal syncope can be a challenging experience, as the condition can be unpredictable and disruptive to daily life. However, there are strategies and lifestyle modifications that individuals can adopt to help manage this condition more comfortably.
Lifestyle Modifications
One of the key ways to reduce the frequency and severity of vasovagal episodes is by making certain lifestyle modifications. Maintaining a well-balanced diet is crucial, as certain foods and beverages can trigger episodes. It is important to avoid consuming excessive amounts of caffeine, alcohol, and high-sodium foods, as they can exacerbate symptoms. Instead, individuals should focus on consuming a diet rich in fruits, vegetables, whole grains, and lean proteins.
In addition to a healthy diet, regular exercise is also important in managing vasovagal syncope. Engaging in moderate-intensity exercise, such as walking, swimming, or cycling, can help improve cardiovascular health and reduce the likelihood of fainting episodes. However, individuals should be cautious and avoid overexertion, as intense physical activity can trigger a vasovagal response.
Managing stress levels is another crucial aspect of living with vasovagal syncope. Stress can act as a trigger for fainting episodes, so it is important to find effective stress management techniques. Deep breathing exercises, meditation, and mindfulness practices can help individuals relax and reduce their overall stress levels. Engaging in activities that promote relaxation, such as yoga or tai chi, can also be beneficial.
Adequate rest and sleep are essential for individuals with vasovagal syncope. Fatigue can increase the likelihood of fainting episodes, so it is important to prioritize getting enough sleep each night. Establishing a regular sleep schedule and creating a relaxing bedtime routine can help improve the quality of sleep and reduce the risk of syncope.
Coping Strategies and Support
Living with vasovagal syncope can be emotionally challenging, as individuals may feel anxious or fearful about experiencing another episode. Receiving support from loved ones and joining support groups can provide individuals with the emotional support and understanding they need. Sharing experiences, learning from others, and exchanging coping strategies can be invaluable in managing the challenges associated with a vasovagal response.
In addition to emotional support, individuals with vasovagal syncope may benefit from medical interventions. Consulting with a healthcare professional who specializes in autonomic disorders can help individuals develop a personalized treatment plan. This may include medications to manage symptoms, such as beta-blockers or selective serotonin reuptake inhibitors (SSRIs), or other interventions like cardiac pacing or tilt table testing.
Furthermore, individuals should always carry identification that indicates their medical condition, such as a medical alert bracelet or card. This can help ensure that in the event of a fainting episode, bystanders and medical professionals are aware of the individual’s condition and can provide appropriate care.
In conclusion, understanding what happens in a vasovagal response is key to managing this common condition effectively. By recognizing the triggers, symptoms, and undergoing a proper medical evaluation, individuals can devise personalized treatment plans to minimize the impact of vasovagal episodes on their daily lives. Living with vasovagal syncope may require lifestyle modifications and the utilization of coping strategies, but with the right support and knowledge, individuals can lead fulfilling lives while effectively managing this condition.