After experiencing a vasovagal episode, it is essential to take the appropriate steps to ensure your well-being and prevent future incidents. Understanding the condition and its triggers is crucial in managing and minimizing the impact it has on your life. In this article, we will discuss the immediate response to a vasovagal episode, the importance of medical evaluation, long-term management strategies, and the emotional impact of living with this condition.
Understanding Vasovagal Syncope
Vasovagal syncope, also known as a vasovagal episode or fainting spell, is a sudden loss of consciousness caused by a temporary drop in blood flow to the brain. It is the most common type of fainting and is typically triggered by emotional stress, pain, or standing up too quickly. The body’s automatic nervous system overreacts, leading to a decrease in heart rate and blood pressure.
When it comes to understanding vasovagal syncope, it is important to delve deeper into its definition and causes. The term “vasovagal” refers to the involvement of the vagus nerve, which plays a crucial role in regulating heart rate and blood pressure. This nerve is responsible for transmitting signals between the brain and various organs, including the heart. When the vagus nerve is stimulated excessively, it can cause a sudden drop in blood pressure and heart rate, leading to a lack of blood flow to the brain and resulting in fainting.
There are several factors that can trigger a vasovagal episode. Emotional stress, such as anxiety, fear, or even excitement, can activate the body’s fight-or-flight response, causing the blood vessels to constrict and reducing blood flow to the brain. Additionally, experiencing pain, whether it be due to an injury or a medical procedure, can also trigger a vasovagal response. This is because the body’s natural response to pain is to lower blood pressure, which can lead to fainting. Furthermore, standing up too quickly can cause blood to pool in the legs, leading to a sudden drop in blood pressure and resulting in a vasovagal episode.
Common Symptoms of a Vasovagal Episode
Recognizing the symptoms of a vasovagal episode is essential for prompt action. While the loss of consciousness is the most obvious symptom, there are several other signs that can indicate an impending episode. Lightheadedness is a common symptom experienced by individuals before fainting. This sensation can be described as feeling dizzy or as if one’s head is spinning. Additionally, individuals may also feel hot or cold, as the body’s temperature regulation can be affected during a vasovagal episode.
Another symptom to watch out for is nausea. Many individuals experience a feeling of queasiness or an upset stomach before fainting. This can be attributed to the body’s response to the sudden drop in blood flow, which can disrupt the digestive system. Blurred vision is another common symptom experienced during a vasovagal episode. Individuals may notice that their vision becomes hazy or that they have difficulty focusing on objects. This is due to the temporary decrease in blood flow to the eyes.
In severe cases, a brief loss of consciousness may occur. This can last for a few seconds to a few minutes. During this time, the individual may appear pale or have a blank expression. It is important to note that while losing consciousness can be alarming, it is usually a temporary and harmless condition. However, it is crucial to seek medical attention if the individual does not regain consciousness or if there are any other concerning symptoms present.
Some individuals may experience warning signs before an episode, such as sweating or feeling anxious. These premonitory symptoms can serve as an early indication that a vasovagal episode is imminent. Paying attention to these warning signs can help individuals take appropriate measures to prevent or manage an episode, such as lying down or sitting with their head between their knees to increase blood flow to the brain.
Immediate Response to a Vasovagal Episode
Steps to Take During a Vasovagal Episode
If you feel an episode coming on, it is crucial to take immediate action to minimize injury and prevent further complications. Vasovagal episodes, also known as fainting spells, occur when there is a sudden drop in blood pressure and heart rate, leading to a temporary loss of consciousness. These episodes can be triggered by various factors, including emotional stress, pain, dehydration, or standing up too quickly.
First, try to lie down or sit with your head between your knees, allowing blood flow to return to the brain. This position helps counteract the drop in blood pressure and can prevent fainting. If unable to lie down, sit down and place your head as close to the ground as possible. By doing so, you can still promote blood flow to the brain and reduce the risk of injury from falling.
In addition to positioning, it is important to loosen any tight clothing that may restrict blood flow. Tight clothing can exacerbate the episode and make it more difficult for your body to recover. By removing any constricting garments, you can help improve blood circulation and potentially alleviate symptoms.
If you are unable to prevent the loss of consciousness, make sure that you are in a safe and open area to prevent injuries from falls. Clear any nearby objects that may pose a risk and ensure that there are no sharp edges or hard surfaces that could cause harm. Taking these precautions can help protect you during the episode and minimize the chances of sustaining injuries.
Post-Episode Care and Recovery
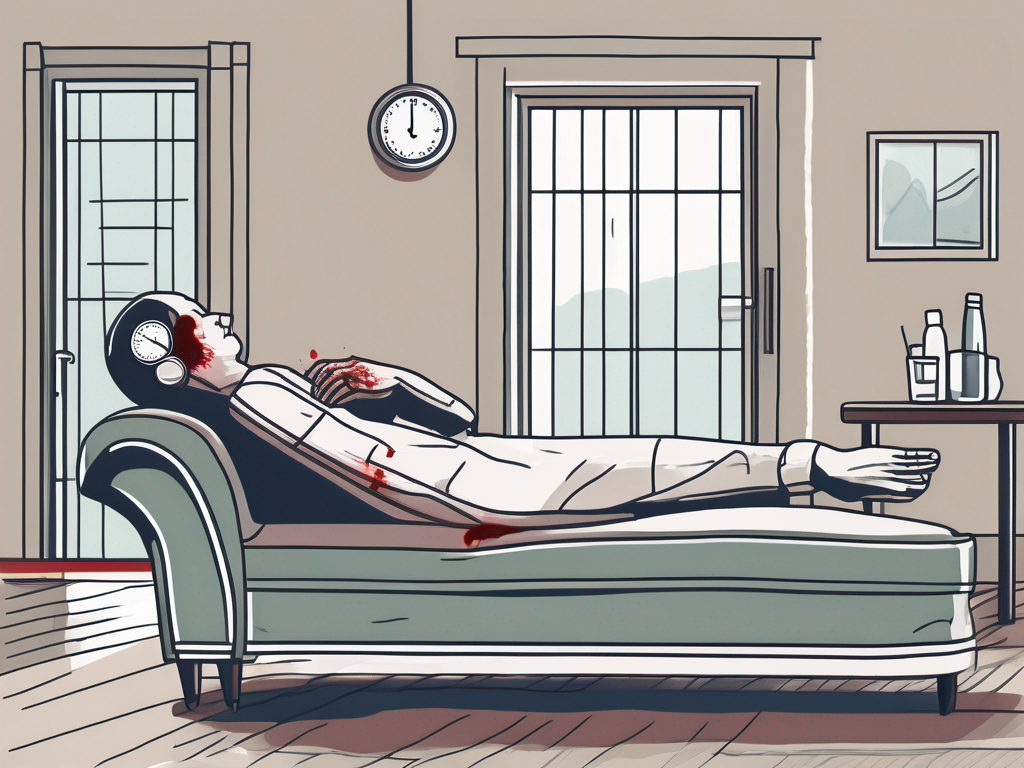
After a vasovagal episode, it is essential to rest and gradually regain your strength. Resting allows your body to recover from the stress it endured during the episode. Lie down in a comfortable position and take deep breaths to help stabilize your breathing and heart rate. It is important to avoid sudden movements or activities that may strain your body.
Make sure to hydrate yourself by drinking water or clear fluids. Dehydration can contribute to the occurrence of vasovagal episodes, so replenishing your body’s fluid levels is crucial. Sip on water slowly and avoid consuming sugary or caffeinated beverages, as they can further dehydrate you.
It is advisable to avoid activities that can trigger another episode, such as standing up for long periods or exposure to extreme temperatures. Take it easy and gradually resume your normal activities once you feel fully recovered. If you experience any lingering symptoms or have concerns about future episodes, consulting with a healthcare professional is advisable.
Speaking to a healthcare professional can help rule out any underlying medical conditions or potential triggers for your vasovagal episodes. They can provide guidance on how to manage future episodes and offer specialized recommendations based on your individual situation. Your doctor may suggest lifestyle modifications, such as increasing your fluid intake, managing stress levels, or avoiding certain triggers.
Remember, while vasovagal episodes can be distressing, they are usually not life-threatening. By taking appropriate measures during an episode and seeking medical advice, you can effectively manage and reduce the frequency of these episodes, allowing you to live a healthy and fulfilling life.
Medical Evaluation After a Vasovagal Episode
When to Seek Medical Attention
If you experience a vasovagal episode for the first time, it is crucial to seek immediate medical attention. This will help determine the underlying cause and rule out any serious health issues that may be contributing to the episode. It is always better to be safe than sorry when it comes to your health. Remember, your well-being is of utmost importance.
When you visit a healthcare professional, they will carefully assess your condition and provide the necessary medical intervention. They have the expertise and knowledge to identify any potential risks or complications that may be associated with your vasovagal episode. Seeking medical attention promptly can help prevent any further complications and ensure that you receive the appropriate treatment.
In addition to seeking medical attention after the first episode, it is also important to consult with a physician if your episodes become more frequent or if they occur under different circumstances than before. This change in pattern could indicate an underlying condition that needs to be addressed. Your doctor will be able to evaluate your symptoms and provide guidance on the best course of action.
What to Expect During a Medical Evaluation
A medical evaluation for vasovagal episodes typically involves a comprehensive assessment of your medical history, a thorough physical examination, and potentially further diagnostic tests. It is essential for your healthcare provider to gather as much information as possible to make an accurate diagnosis and develop an appropriate treatment plan.
During the evaluation, your doctor will inquire about any triggers or warning signs you have experienced before or during the episodes. This information will help them understand the specific circumstances that may be contributing to your vasovagal episodes. By identifying these triggers, your doctor can provide you with strategies to avoid or manage them effectively.
In addition to the medical history, your healthcare provider will perform a physical examination to assess your overall health. This examination may involve checking your blood pressure, heart rate, and other vital signs. It allows your doctor to evaluate your physical well-being and identify any abnormalities that may be related to your vasovagal episodes.
Depending on your specific case, your doctor may also recommend further diagnostic tests to gain a more in-depth understanding of your condition. These tests may include blood tests to check for any underlying medical conditions, an electrocardiogram (ECG) to assess your heart’s electrical activity, and tilt-table testing to evaluate your body’s response to changes in position.
By conducting these tests, your healthcare provider can gather valuable information to aid in the diagnosis and treatment of your vasovagal episodes. It is important to cooperate fully with your doctor and follow their instructions throughout the evaluation process. This will ensure that you receive the most accurate diagnosis and appropriate care for your condition.
Long-Term Management of Vasovagal Syncope
Lifestyle Changes to Prevent Vasovagal Episodes
While there is no guaranteed way to prevent vasovagal episodes, making certain lifestyle adjustments can significantly reduce their frequency. Staying well-hydrated and maintaining a healthy diet are essential.
When it comes to staying hydrated, it’s not just about drinking enough water. Electrolyte balance is crucial for maintaining proper nerve and muscle function. Including foods rich in electrolytes, such as bananas, avocados, and coconut water, can help replenish these essential minerals.
Additionally, a healthy diet can support overall cardiovascular health. Consuming foods that are low in sodium and saturated fats while high in fiber, antioxidants, and omega-3 fatty acids can help regulate blood pressure and reduce the risk of heart disease.
Avoiding triggers is another important aspect of managing vasovagal syncope. Prolonged standing can lead to blood pooling in the lower extremities, triggering a vasovagal response. Taking breaks, shifting weight from one leg to another, or using compression stockings can help improve blood circulation and prevent episodes.
Extreme heat can also be a trigger for vasovagal syncope. It’s important to stay cool and hydrated in hot environments, especially during physical activities or exposure to direct sunlight. Wearing lightweight, breathable clothing and using fans or air conditioning can help regulate body temperature.
Stress management techniques can also play a significant role in preventing vasovagal episodes. Engaging in relaxation exercises, such as deep breathing, meditation, or yoga, can help reduce stress levels and promote overall well-being. Finding healthy outlets for stress, such as hobbies or support groups, can also be beneficial.
Regular exercise, particularly cardiovascular exercises that enhance autonomic nervous system function, may be beneficial. However, it is important to consult with your healthcare provider before starting any new exercise regimen.
Medical Treatments and Interventions
In some cases, medical treatments or interventions may be necessary to manage vasovagal syncope effectively. Your doctor may recommend medications, such as beta blockers or selective serotonin reuptake inhibitors (SSRIs), to help regulate your autonomic nervous system.
Beta blockers work by blocking the effects of adrenaline, reducing heart rate and blood pressure. This can help prevent the sudden drop in blood pressure that triggers a vasovagal episode. SSRIs, on the other hand, can help regulate serotonin levels in the brain, which may have a positive impact on the autonomic nervous system.
In more severe cases, pacemakers or other devices may be considered for individuals with recurrent episodes that significantly impact their quality of life. These devices can help regulate heart rate and rhythm, providing a more stable cardiovascular system.
It’s important to work closely with your healthcare provider to determine the most appropriate treatment plan for your specific situation. Regular follow-up appointments and open communication can help ensure that your management plan is effective and tailored to your needs.
Emotional Impact of Vasovagal Syncope
The emotional impact of living with vasovagal syncope can be significant. Anxiety and fear-related to the potential for future episodes and their unpredictable nature are common. The fear of losing consciousness or experiencing an episode in public can lead to a constant state of worry and apprehension. This can affect a person’s overall quality of life, causing them to limit their activities and social interactions.
Engaging in stress-management techniques can help alleviate these emotional challenges. Deep breathing exercises, for example, can help calm the mind and body during moments of anxiety. By focusing on slow, controlled breaths, individuals can reduce their heart rate and promote a sense of relaxation. Mindfulness practices, such as meditation or yoga, can also be beneficial in managing anxiety and promoting emotional well-being.
Therapy can play a crucial role in coping with the emotional impact of vasovagal syncope. Speaking with a mental health professional can provide individuals with a safe space to express their fears and concerns. Therapists can offer guidance and support, helping individuals develop coping mechanisms and strategies to manage their anxiety. Cognitive-behavioral therapy, in particular, has been shown to be effective in helping individuals reframe negative thoughts and develop healthier ways of managing stress.
In addition to individual therapy, support groups or online communities can provide a valuable source of support. Connecting with others who are facing similar experiences can help individuals feel less alone and isolated. Sharing stories, tips, and advice can provide a sense of camaraderie and understanding. These communities can also serve as a platform for individuals to learn from one another and discover new coping strategies.
Coping with Anxiety and Fear
Living with vasovagal syncope often means coping with anxiety and fear. The fear of experiencing a sudden episode can be overwhelming, leading to heightened levels of stress and worry. It is important for individuals to develop effective coping mechanisms to manage these emotions.
One strategy is to practice relaxation techniques regularly. Deep breathing exercises, where individuals take slow, deep breaths and focus on their breath, can help calm the nervous system and reduce anxiety. Progressive muscle relaxation, where individuals tense and then relax different muscle groups, can also promote a sense of relaxation and reduce stress.
Mindfulness is another helpful technique for managing anxiety and fear. By staying present in the moment and focusing on the sensations of the body or the environment, individuals can redirect their attention away from anxious thoughts. Mindfulness meditation, guided imagery, and body scans are all practices that can be incorporated into a daily routine to promote emotional well-being.
Therapy can also be an effective tool for coping with anxiety and fear related to vasovagal syncope. Cognitive-behavioral therapy (CBT) is a commonly used approach that helps individuals identify and challenge negative thought patterns. By reframing negative thoughts and replacing them with more positive and realistic ones, individuals can reduce their anxiety and improve their overall well-being.
Support groups or online communities can provide a valuable source of support for individuals coping with anxiety and fear. Connecting with others who are facing similar experiences can help individuals feel understood and less alone. Sharing experiences, tips, and coping strategies can provide a sense of camaraderie and empowerment.
Building a Support System for Vasovagal Syncope Management
Building a support system is crucial for managing the impact of vasovagal syncope on your daily life. Educating your close friends, family members, and coworkers about your condition is essential so that they can provide understanding and assistance when needed. By explaining the nature of vasovagal syncope, its triggers, and the potential symptoms, you can help others better comprehend your experiences.
Consider sharing information about your condition, triggers, and emergency protocols with those closest to you. This can help them recognize the signs of an impending episode and respond appropriately. It is also important to discuss any specific actions that can help during an episode, such as laying the person flat or elevating their legs to improve blood flow to the brain.
In some cases, it may be beneficial to carry a medical alert card or wear a medical bracelet that indicates your condition. This can serve as a visual reminder for others to be aware of your condition in case of an emergency. Medical professionals and first responders can quickly identify your condition and provide appropriate care.
Building a support system also involves seeking professional help. Consulting with a healthcare professional who specializes in vasovagal syncope can provide personalized guidance and recommendations tailored to your individual needs. They can help you develop a comprehensive management plan that includes lifestyle modifications, medication, and other interventions to reduce the frequency and severity of episodes.
In conclusion, understanding how to respond to a vasovagal episode, seeking medical evaluation, implementing long-term management strategies, and addressing the emotional impact of the condition are essential for individuals living with vasovagal syncope. By taking the appropriate steps, you can gain control over your condition and minimize its impact on your daily life. Remember to consult with a healthcare professional for personalized guidance and recommendations tailored to your individual needs.